Everyone has their own unique sets of strengths and challenges and there are a variety of additional factors that contribute to the distinctive complexities associated with FASD, including the social determinants of health, intergenerational impacts, compounding stigma, environmental adversity, co-occurring mental health issues, and unique caregiver and family experiences1. Understanding some of the common challenges and strengths associated with this disability can help us to work from an FASD-informed perspective. However, when supporting an individual with FASD, it is important to come to understand each person’s individual needs and capabilities. This section will discuss:
Areas of Strengths
Beyond simply recognizing that individuals with FASD have areas of strength (although this is an important first step given the prominent deficit-focused perspective in care), we must also build upon and leverage these strengths. When we do not explore and utilize these strengths, it can continue to reinforce challenges for individuals with FASD with self-esteem and can exacerbate the shame that many individuals with FASD already experience.
In the following video, Myles Himmelreich discusses the focus that is typically faced on deficits when discussing FASD and expresses that his difficulties and diagnosis do not define him.
People with FASD possess a myriad of strengths. This list is not exhaustive and it is important to discuss with the people you support what strengths and capabilities they have that can be leveraged to achieve their goals2,3.
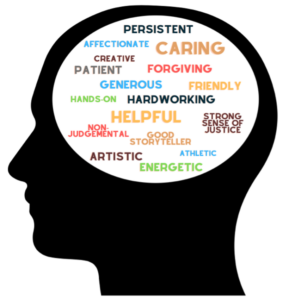
Flannigan and colleagues (2021) highlighted the following strengths for people with FASD in their research, which are important considerations in the context of mental health support:
- Strong self-awareness
- Receptiveness to support
- Capacity for human connection
- Perseverance through challenges
- Hope for the future
These capabilities are vitally important in the context of mental health therapy and support and can be built upon and used to increase wellbeing. Creating opportunities to actualize these strengths may help to support a heightened sense of wellbeing and happiness.
For additional information on working from a strengths-based perspective, see Section 7.
Areas of Challenge
There has been significant research examining the potential difficulties associated with FASD which fall into the following categories: motor skills, cognition, language and communication, academic achievement, learning and memory, attention, executive functioning, affect regulation, and adaptive/social skills4 (for more information on FASD diagnosis please see Section 5). The impact of these difficulties will be different for everyone but may result in a variety of challenges such as inconsistent memory/recall problems, challenges with sensory processing, decreased mental stamina, difficulty interpreting abstract concepts, impulsivity, difficulty shifting from one context to another, resistance to change, and challenges in picking up on social cues.
It is also important to note that FASD is a “whole-body diagnosis”, and many individuals will struggle with a range of physical health problems at far higher rates than the general population5,6. These physical health problems are an important consideration for social workers and mental health professionals who may need to support their clients with health-related issues (e.g., organizing appointments or understanding/taking medications)5.
Click on each of the dropdown options below to learn more about areas of challenges.
An important consideration regarding FASD is a common pattern of uneven development across areas of functioning. For example, an 18-year-old may speak and express themselves like a typically developed 20-year-old, have the social skills of a 7-year-old, the life skills of an 11-year-old, and read like a 16-year-old. People’s functioning will vary across aspects of functioning and development and so it is important to recognize that just because someone may appear to have a strength in one area, does not mean they do not need support in others.
Research in FASD has found that individuals may have limitations in cognitive development and functioning. These limitations can include having a lower IQ (intellectual functioning), challenges with executive functioning, academic achievement, and motor functioning as well as difficulties with learning, memory, and visual-spatial abilities.
Challenges with executive functioning are common for individuals with FASD and can include difficulties with planning, decision-making, inhibition, working memory, flexible thinking, strategy use, cause-effect reasoning, fluency, and behaviour regulation7,8. These difficulties will likely require flexibility and adaptability in mental health practice, and being FASD-informed to meet people where they are.
In the video above, Megan from the Lakeland Centre for FASD explains executive functioning: FASD & Executive Functioning Explained
In the video above, Kara Hurley and her mother discuss a real-world example of struggles with executive functioning: Executive Functioning and Adolescents with FASDs
Adaptive functioning refers to skills related to daily living that are based on developmental and sociocultural standards related to independence and responsibility9. There are three areas of adaptive skills: social (e.g., communication, relationship development), practical (e.g., grooming, dressing, eating), and conceptual (e.g., reading, writing).
Social functioning may be a challenge for some individuals with FASD, and this difficulty may also increase with age, which is why intervention and support is important9,10. Some common experiences for people with FASD in social situations can include inappropriate responses, difficulties getting along with peers (e.g., exclusion, teasing), and problems developing and maintaining relationships.
Individuals with FASD may have challenges with expressive and receptive language skills. There can sometimes be a tendency to be talkative and expressive, but it may be challenging for others to understand the meaning of the exchange11. Some individuals with FASD may be able to paraphrase what is said to them, but they may not demonstrate full comprehension of the topic or idea11. These are just some examples of language and communication challenges that have been highlighted in research, but language skills will vary greatly among individuals.
In the following video Myles Himmelreich shares information about physical challenges that can be associated with FASD: FASD: Physical Challenges
Individuals with FASD may have challenges with aggressive behaviours. Watch this CanFASD webinar recording to learn about the conceptualization of aggressive behaviours and FASD. The following resources may also be useful to families and service providers looking for support with helping an individual who is showing signs of aggressive behaviours –
Reframing Behaviour
When supporting individuals with FASD it is important to be informed about the strengths and challenges people may have. Reframing challenging behaviour can be an integral part of adapting one’s practice to the unique needs of each person with FASD. Mental health professionals may initially perceive difficulties or a lack of change as intentional, a lack of motivation, or a lack of effort instead of seeing needs that require support and flexibility of approach. Reframing challenging behaviour allows you to assess needs, strengths, and strategies to better support someone.
Download Handout
The following handout has examples of behaviour you may see in your mental health practice, and how to reframe them from a FASD-informed perspective. FASD and Mental Health: Reframing Behaviour.
FASD Throughout the Lifespan
Prenatal alcohol exposure and a diagnosis of FASD can have impacts on a person throughout their life. It is important to understand that as we all grow up our capacities and goals will change. FASD can have impacts from birth, with biological and genetic vulnerabilities that can then be exacerbated by behavioural, social, and environmental factors as one grows up12. As mental health professionals, reflecting on the specific developmental capacities of our clients, as well as how this continues to be influenced by one’s life experiences, is important in adapting our practices for success. We need to consider the individual holistically and across time9.
The following are areas of challenges and behaviours that people with FASD may experience across their lifespan.
Childhood
- Developmental delays (e.g., in language, motor skills, physical growth, etc.)
- Issues with emotional and behavioural regulation, activity level, and response to overstimulation
- Social difficulties (e.g., being overly friendly, not understanding social cues, communication challenges, difficulty making friends)
- Challenges moving from concrete to abstract concepts
- Lack of focus, and hyperactivity (e.g., difficulty with unstructured time)
- Not learning from consequences
Without the understanding of brain-based differences as well as the vulnerability to negative life experiences, unrealistic/inappropriate expectations of behaviour and ability can continually set children up for failure. It is important to take a life course approach and recognize that transitions and experiences can greatly impact the trajectories for children and youth13. Appropriate support and interventions that consider the influence of adverse experiences, cognitive, behavioural, and socio-emotional functioning is important to respond appropriately and effectively12.
In childhood, challenges within cognition, learning and memory, attention, and academic achievement may begin to be observed14. It has also been found that children with FASD may have an increased rate of mood disturbances such as depressive symptoms as well as oppositional defiant disorder, conduct disorder, and ADHD7.
It is also important to recognize that children with FASD are more vulnerable to experience abuse, neglect, challenges in education, involvement with the criminal justice system, co-occurring mental health conditions, alcohol and substance use, and are also overrepresented in the child welfare system13. In 2019, Cook and colleagues reported that at least 3-11% of children in the child welfare system have FASD (the general population rate of FASD is 2-4%). It is a common adverse experience for people with FASD to have unstable home placements and caregiver disruptions13. However, having a stable and nurturing home environment is an integral protective factor for individuals with FASD13,15. It is therefore important to consider the larger caregiver/familial environment when working with children with FASD.
Adolescence
- Increasing behavioural and emotional regulation difficulties
- Challenges with critical thinking, abstract thinking and judgment skills
- A lack of connection between thoughts, feelings and actions
- Potential challenges in school (e.g., disruption, getting in trouble), involvement with the law, and/or sexually inappropriate behaviour
- Issues with self-esteem, impulsivity, and motivation
- Heightened risk of mental health challenges and substance use concerns
- Difficulty resisting negative peer influences
- May have trouble with accurately interpreting social cues (e.g., words, actions, non-verbal cues)
Adolescence and teenage hood present its own unique challenges for individuals, families, and caregivers. Without identification and support, challenges from childhood are likely to be exacerbated and impacted by changing biology and social expectations. It is also important to remember that, as mentioned previously, FASD can result in uneven development, and so an adolescent may be skilled, and talented in some areas but need significant support in others. This discrepancy can sometimes result in a misinterpretation of teenage behaviour as lazy or unmotivated rather than seeing it as an area of need.
Adolescents also have significant strengths and have a desire for their unique characteristics to be recognized and appreciated16. Children and adolescents have reported challenges with anxiety which can impact independence and confidence and may lead to becoming socially isolated or struggling to engage in school16. Therefore, promoting positive relationships and developing coping mechanisms for anxiety may be important practice considerations for mental health professionals. When supporting teenagers and adolescents, it may also be important to engage with the family and/or caregivers.
Adults
- Potential difficulties with education (e.g., attainment, disruption) as well as employment
- Challenges with independent living and adaptive skills (e.g., self-care, money management, social communication, relationships)
- Social skill issues (e.g., difficulties with communication and/or developing relationships)
- Co-occuring mental health challenges/diagnoses are likely (e.g., anxiety, depression, ADHD)
- Potential to withdraw or self-isoalte
People with FASD when not supported or provided with appropriate interventions can have an increased vulnerability to encounter negative life experiences as adults such as challenges with independent living and employment, involvement with the law, confinement due to mental health, and problems with sexually inappropriate behaviour15. For example, 11-23% of youth and 10-18% of adults in correctional settings were reported to have FASD (compared to 2-4% in general population)17. It is important to consider the intersecting challenges and life experiences that may affect adults with FASD who are accessing mental health support. The variation of difficulties in multiple areas also speaks to the need for a multidisciplinary and collaborative approach to care.
Download Resources
- For a downloadable handout on the basics of FASD that can be given to individuals who have FASD and their families, please click here: General Information About FASD
- The following resource may be helpful as a guide for parents and caregivers on how they can explain a diagnosis of FASD to their child: How to Explain an FASD Diagnosis to Your Child
Becoming a Parent
Becoming a parent is a pivotal moment for anyone, filled with demands and a need for support. The skills and abilities of parents are constantly evolving, including for parents with FASD9. Canadian estimates of the number of parents living with FASD are generally around 300,00018. People with FASD who become parents may also face a variety of personal challenges that impact their ability to parent such as difficulties with memory, organization, and integrating sensory cues as well as systemic barriers such as societal attitudes, scrutiny of parenting, and subsequent anxiety and feelings of inadequacy9.
These challenges may also be exacerbated by adverse life experiences (e.g., trauma, abuse, entanglement with criminal justice or child welfare systems), lack of support, and isolation19, 11. Mental health providers should consider the ways in which the social determinants of health, access to health care, education, and employment also impact individuals with FASD19.
Abraham (2005) identified the most pressing needs of parents with FASD to be20:
- Support with the practical and domestic skills required to care for children
- Training on parental skills and child development
- Assistance with obtaining public and social service
- Formal and informal relational support
Some strategies to support parents may include developing appropriate coping mechanisms, discussing parenting strategies, and identifying a safety net of support for the individual and family (including people, programs, resources)11. Parents have also identified effective strategies including the frequent use of a calendar, highly detailed instructions, having a consistent routine, taking time for themselves, and focusing on positive behaviours of their children18. In addition, it may be important for a parent with FASD to have a relationship with a parental mentor who can support navigating common behaviours and experiences as it can be helpful to understand and see how other people navigate parenting and relationships.
However, it is also important to consider that although improving parenting skills may be an important goal for parents with FASD, this improvement should be considered in the context of first addressing urgent needs such as safety, stable housing, food security, financial stability, and mental health and substance use treatment21, 19.
SUPPORT AREA
HOW TO SUPPORT
Sexual health, contraception, and education around the risks of drinking when pregnant
- People with FASD who wish to have children should be offered appropriate sexual health and contraception information
- Education about the risks of alcohol and substance use during pregnancy
Basic needs
- Help in accessing safe and stable housing
- Education and support regarding self-care (e.g., nutrition)
- Mental health support
Supportive mentorship
- Advocate for and connect individuals with community resources
Strengths-based support
- Actively consider the strength and resiliency of individuals of FASD
- Engage in reflection to provide non-judgmental and non-stigmatizing support
FASD-informed
- Continued education about FASD
Sex-Related Differences
Considering the sex and gender related differences in health and wellbeing can be important in understanding and supporting people with developmental disabilities. There is limited research on sex and gender related differences for people with FASD, as well as research that highlights the experiences and lived realities of FASD for gender-diverse people.
A recent study aimed to inform the practice of service providers working with people with FASD/prenatal alcohol exposure, with attention on exploring the overlapping and differing needs and experiences of males and females. The findings highlighted that there were no significant differences for FASD diagnostic outcomes or physical indicators of prenatal alcohol exposure22.
However, there were important differences with males experiencing significantly more neurodevelopmental impairment, high rates of ADHD, conduct disorder, and oppositional defiance disorder, and females experiencing higher rates of endocrine problems, anxiety, and depressive/mood disorders22.
There were also differences in terms of adversity, with males experiencing more difficulties with school and offending/incarceration and females experiencing higher rates of trauma and legal problems with victimization and custody22.
However, the authors also note that, “the dichotomous distinction between male and female can oversimplify the complex, nuanced, and dynamic interactions between sex and gender and related life experiences, as well as the broader…sociocultural factors”22. As such, additional research is needed that explores the intersections of sex, gender, and FASD. Unfortunately, there is currently limited evidence and research regarding the experiences of people with FASD and those who identify as having diverse sexual orientations, gender identities, and gender expressions. See Gap Analysis: Sexual Orientation, Gender Identity, Gender Expression, and FASD.
As a mental health professional, it is important to consider and reflect on how the sex and gender identity of the client you are supporting may impact their experiences of violence, trauma, mental and physical health.
FASD and Families
There is a vast spectrum of family types who are raising youth with FASD, as many children with FASD may not reside with their birth families but may be raised in adoptive or foster settings, with grandparents or great-grandparents, with other extended family members, kinship networks, etc. and FASD can have a large impact on everyone in the family unit23,1. Receiving a diagnosis of FASD can be difficult to access (especially as an adult), may be costly, and common challenges of FASD may not be prominent enough to seek out a diagnosis23. Without a diagnosis children and families can be left without the help they require, and many caregivers will continue to play a support role for their children well into adulthood because of the lack of services1.
Parents of children with FASD can experience a range of emotional reactions and challenges including stress, social isolation, feeling misunderstood, and being blamed by service providers for the challenges of their children23,1. Parents have also reported that having a child with FASD can impact their other children, as well as relationships with extended family members23. There is generally a lack of understanding and knowledge regarding FASD in society, as well as in social services and support, which can result in a lack of assistance and understanding for parents23.
Download Resources
- The FASD Support Network of Saskatchewan has developed strategies for parents and caregivers supporting people with FASD: FASD Tips for Parents and Caregivers
- CanFASD has developed a caregiver resource guide for those providing care to persons with FASD: Caregiver Resource Guide
- Healthy Child Manitoba developed a resource on information for parents and caregivers regarding FASD: What Parents and Caregivers Need to Know About FASD
Final Thought
The following video captures what a group of adults and young people living with FASD wish people knew and speaks to many of the ideas discussed above: What I wish people knew about me – living with FASD.
Download Handout
For a summary of information, download the Mental Health Resource and Practice Guide Section 2 Summary.
References
1Flannigan, K., Pei, J., McLachlan, K., Harding, K., Mela, M., Cook, J., Badry, D., & McFarlane, A. (2022a) Responding to the Unique Complexities of Fetal Alcohol Spectrum Disorder. Frontiers in Psychology. https://doi.org/10.3389/fpsyg.2021.778471
2Flannigan, K., Harding, K., Reid, & Family Advisory Committee. (2018). Strengths Among Individuals with FASD. Vancouver (BC): CanFASD.
3Flannigan, K., Wrath, A., Ritter, C., McLachlan, K., Harding, K. D., Campbell, A., … & Pei, J. (2021). Balancing the story of fetal alcohol spectrum disorder: A narrative review of the literature on strengths. Alcoholism: Clinical and experimental research, 45(12), 2448-2464. https://doi.org/10.1111%2Facer.14733
4Cook, J. L., Green, C. R., Lilley, C. M., Anderson, S. M., Baldwin, M. E., Chudley, A. E., … & Rosales, T. (2016). Fetal alcohol spectrum disorder: a guideline for diagnosis across the lifespan. Cmaj, 188(3), 191-197. https://psycnet.apa.org/doi/10.1503/cmaj.141593
5Himmelreich, M., Lutke, C. J., & Hargrove, E. T. (2020). The lay of the land: Fetal alcohol spectrum disorder (FASD) as a whole-body diagnosis. In The Routledge handbook of social work and addictive behaviors (pp. 191-215). Routledge.
6Mela, M., Coons-Harding, K. D., & Anderson, T. (2019). Recent advances in fetal alcohol spectrum disorder for mental health professionals. Current Opinion in Psychiatry, 32(4), 328-335. https://doi.org/10.1097/yco.0000000000000514
7Mattson, S. N., Crocker, N., & Nguyen, T. T. (2011). Fetal alcohol spectrum disorders: neuropsychological and behavioral features. Neuropsychology review, 21, 81-101. https://doi.org/10.1007%2Fs11065-011-9167-9
8Rasmussen, C., & Bisanz, J. (2009). Executive functioning in children with fetal alcohol spectrum disorders: profiles and age-related differences. Child Neuropsychology, 15(3), 201-215. https://doi.org/10.1080/09297040802385400
9Pei, J., Kapasi, A., Kennedy, K.E., & Joly, V. (2019). Towards Healthy Outcomes for Individuals with Fetal Alcohol Spectrum Disorder. Canada FASD Research Network in collaboration with the University of Alberta.
10Kully‐Martens, K., Denys, K., Treit, S., Tamana, S., & Rasmussen, C. (2012). A review of social skills deficits in individuals with fetal alcohol spectrum disorders and prenatal alcohol exposure: profiles, mechanisms, and interventions. Alcoholism: Clinical and Experimental Research, 36(4), 568-576. https://doi.org/10.1007/s10597-010-9342-0
11Wemigwans, J. (2008). FASD Tool Kit for Aboriginal Families. Ontario Federation of Indian Friendship Centres.
12Flannigan, K., Coons‐Harding, K. D., Anderson, T., Wolfson, L., Campbell, A., Mela, M., & Pei, J. (2020). A systematic review of interventions to improve mental health and substance use outcomes for individuals with prenatal alcohol exposure and fetal alcohol spectrum disorder. Alcoholism: Clinical and Experimental Research, 44(12), 2401-2430. https://doi.org/10.1111%2Facer.14490
13Badry, D., & Harding, K. (2020). Fetal Alcohol Spectrum Disorder and Child Welfare. Vancouver (BC): CanFASD.
14Rasmussen, C., Horne, K., & Witol, A. (2006). Neurobehavioral functioning in children with fetal alcohol spectrum disorder. Child Neuropsychology, 12(6), 453-468. https://doi.org/10.1080/09297040600646854
15Streissguth, A. P., Bookstein, F. L., Barr, H. M., Sampson, P. D., O’malley, K., & Young, J. K. (2004). Risk factors for adverse life outcomes in fetal alcohol syndrome and fetal alcohol effects. Journal of Developmental & Behavioral Pediatrics, 25(4), 228-238. https://doi.org/10.1097/00004703-200408000-00002
16Skorka, K., Copley, J., McBryde, C., Meredith, P. J., & Reid, N. (2022). Lived experiences of adolescents with fetal alcohol spectrum disorder. Developmental Medicine & Child Neurology, 64(12), 1547-1555. https://doi.org/10.1111/dmcn.15290
17Cook, J. (2019). The National FASD Database Winter Update. [Unpublished report].
18Rutman, D., & Van Bibber, M. (2010). Parenting with fetal alcohol spectrum disorder. International Journal of Mental Health and Addiction, 8, 350-361.
19Harding, K. D., Flannigan, K., McFarlane, A., & Reid, D. Parenting with Fetal Alcohol Spectrum Disorder: Needs, Challenges, and Opportunities for Support and Research. Vancouver (BC): CanFASD.
20Abraham, V. (2005). An Investigation Into the Needs of Parents with Fetal Alcohol Spectrum Disorder (FASD). Doctoral dissertation, University of Northern British Columbia).
21Denys, K., Rasmussen, C., & Henneveld, D. (2011). The effectiveness of a community-based intervention for parents with FASD. Community Mental Health Journal, 47, 209-219. https://doi.org/10.1007/s10597-009-9273-9
22Flannigan, K., Poole, N., Cook, J., & Unsworth, K. (2023). Sex‐related differences among individuals assessed for fetal alcohol spectrum disorder in Canada. Alcoholism: Clinical and Experimental Research. https://doi.org/10.1111/acer.15017
23Domeij, H., Fahlström, G., Bertilsson, G., Hultcrantz, M., Munthe‐Kaas, H., Gordh, C. N., & Helgesson, G. (2018). Experiences of living with fetal alcohol spectrum disorders: a systematic review and synthesis of qualitative data. Developmental Medicine & Child Neurology, 60(8), 741-752. https://doi.org/10.1111/dmcn.13696
