Although you may not be involved in the assessment and diagnosis of FASD, it is important to understand the impact that the process of a diagnosis can have on someone and how you can support an individual who you may believe has FASD but does not have a diagnosis. Receiving an early diagnosis can be an integral step toward fostering positive outcomes for people with FASD, so that appropriate interventions and support can be put into place early1. This section will discuss:
FASD as a Diagnosis
According to the most up to date diagnostic guidelines there are two diagnostic labels for individuals with FASD: FASD with sentinel facial features, and FASD without sentinel facial features. There is also a non-diagnostic category: “at risk for neurodevelopmental disorder and FASD with prenatal alcohol exposure”, that indicates that the individual does not currently meet diagnostic criteria but requires future follow-up, as well as support2. There have been a variety of other diagnostic labels over the years that you may come across in other research/resources or that people have previously been diagnosed with, including Fetal Alcohol Syndrome (FAS), partial Fetal Alcohol Syndrome (pFAS), and Alcohol Related Neurodevelopmental Disorder (ARND).
An FASD diagnosis is only made when there is evidence of severe impairment in three or more of the ten neurodevelopmental domains2:
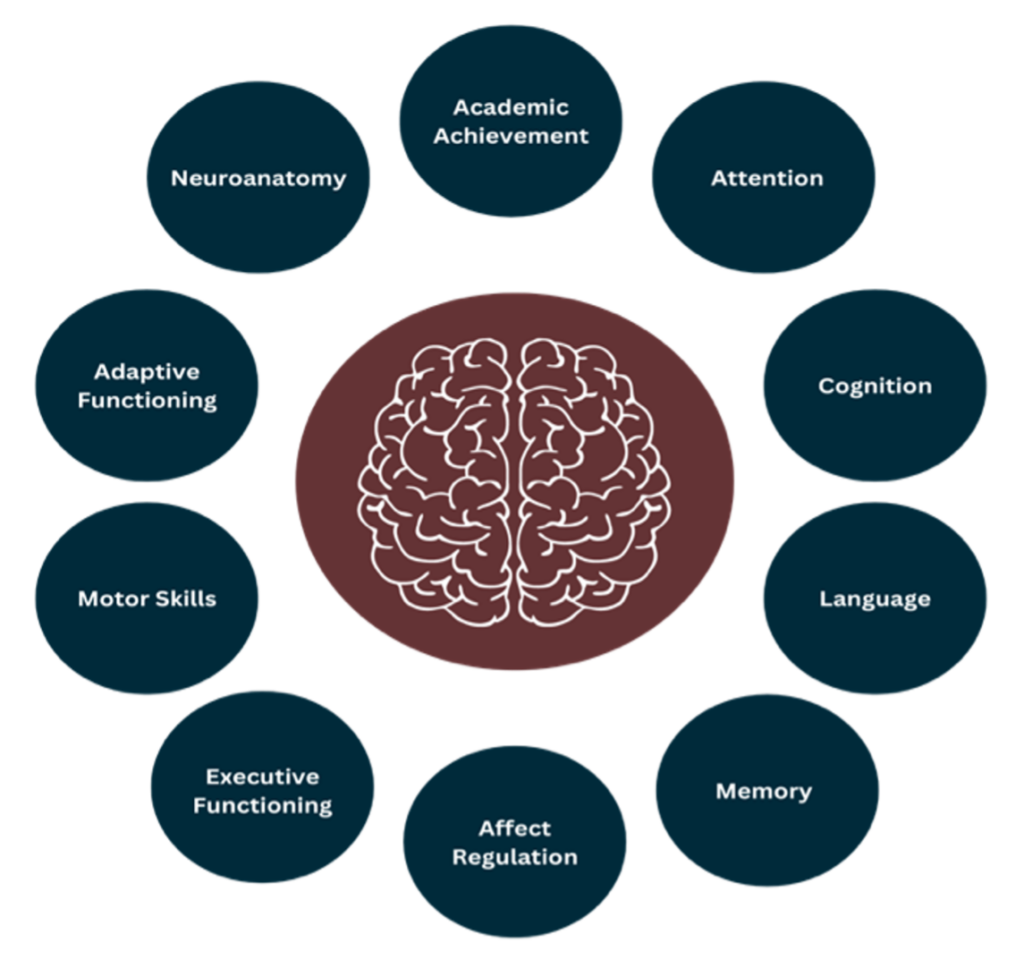
One of the reasons why FASD will look so unique for each person is that the brain domains affected will be different. As mentioned previously, a person needs to score as “severely impaired” in three of the ten brain domains to receive a diagnosis of FASD. However, the three domains that are impacted will be different for everyone, meaning the presentation of FASD will be different and unique for each person.
As a frontline mental health worker, you may be involved in supporting individuals and families through the process of receiving a diagnosis. It is always important to recognize when a client may need to be referred for an FASD assessment.
Identifying People Who May Have FASD
In the context of providing mental health support for individuals with FASD, it is also important to consider how people can be more easily identified in this context. Some organizations may already have an approach in place (e.g., asking about diagnoses at intake or asking FASD-informed questions during initial sessions), but this approach may not be the case and as such it is worth considering how you can identify individuals who may have FASD3. Identification practices can include a range of formal and informal approaches from having a conversation about FASD and asking FASD-informed questions to implementing the use of an FASD screening tool.
Possible FASD-Identification Strategies
Improving FASD identification in mental health practices is important in understanding clients’ strengths and needs. Becoming FASD-informed is an important foundational strategy to better recognize and address the needs of people with FASD3. It is also imperative that FASD-identification is set in a foundation of having plans in place to support clients that are identified as potentially having FASD3. However, if your client is not interested in discussing this or does not wish to answer questions pertaining to FASD, that is okay! You can still discuss strengths, areas of challenge, goals, and ways to best support the individual.
Strategies for Identifying FASD in Mental Health Practice.
The following strategies are adapted from the Moving Towards FASD-Informed Care in Substance Use Treatment guide.
| Strategy | How this could look | Considerations |
| Incorporate brief questions about FASD into existing intake processes | 1. Questions about FASD added to referral or intake forms
2. FASD-informed questions added to intake interviews (with individuals or caregivers, support persons, etc.) 3. Asking questions about FASD once rapport has been built with the client |
Consider what the best time to ask questions is, providing opportunities to circle back to the topic.
Adopting a “universal” approach where all clients are asked initial questions about FASD may help to ensure that no one is missed.
Asking FASD questions at the beginning of support can help with planning accommodations and adaptations. |
| Inviting conversations about FASD with clients | 1. Having curious conversations about FASD with clients
2. If wanted, share information about FASD from a destigmatizing, humanizing, and person-centred approach 3. Engage in conversations about strengths and areas of support (e.g., what has helped in the past) |
Asking direct and respectful questions in the context of a developed relationship is helpful when discussing FASD.
Thoughtfully consider when and with whom to have conversations about FASD.
Consider your own biases as some groups may be incorrectly assumed to have FASD more than others |
| Reviewing records | 1. It may be helpful to review records (e.g., school, social services, health) with consent from the person you are supporting to look for common indicators of FASD | This may inform further conversations about FASD and guide additional screening/assessment.
Information from records may suggest areas of strength and need.
It is also worth considering if meeting the person first is better than getting to know them initially from a file. |
Approaching Clients about FASD
The idea of discussing FASD may feel daunting or uncomfortable initially, but your approach and relationship can facilitate a dialogue that is destigmatizing and informative for support. There are some important components that can help enable a productive and supportive conversations4:
- Establish trust and rapport to create a safe and comfortable space that is non-judgmental.
- Gradually introduce the idea of FASD
- Provide information about FASD that is clear, concise and easy to understand by using simple language and not jargon.
- Ask open ended questions that encourage people to share their ideas and experiences and avoid leading questions.
- Remind people that the diagnosis could help to identify a source of many challenges
- Focus on strengths and abilities and how a diagnosis can support deeper understanding.
- Never assign blame
- Discuss common misconceptions around FASD
Screening Tools
There are a variety of FASD screening tools available; unfortunately, many do not have significant research and evidence validating them in mental health settings. However, there are two screening tools that do have some evidence within mental health and substance use support contexts, as well as in criminal justice system settings (where there would be significant mental health needs), that may be useful in the context of mental health support. The table below outlines these screening tools.
Potential Screening Tools to Identify People who May Have FASD:
The following table is adapted from the Moving Towards FASD-Informed Care in Substance Use Treatment guide.
| Screening Tool | Format | Item Content | Population & Setting Developed For |
| Life History Screen Interview | 27 questions in a semi-structured face-to-face interview | Prenatal alcohol exposure, neurodevelopment and behaviour, life events, mental health | Adult women and men in substance use treatment settings |
| FASD Screening and Referral Tool for Youth Probation Officers | 10-item checklist (i.e., indicating if something is present) completed through chart review and self-report | Prenatal alcohol exposure, growth impairment, neurodevelopment, life events, mental health | Youth on probation (has been used with adults in forensic, community, and correctional settings) |
After Identification
The purpose of outlining some strategies and approaches for identification is to become aware of individuals who may benefit from FASD-informed adaptations to practice, and who may need to be referred for a diagnostic assessment. However, it is important that identification and screening is the first step and that you have a plan in place to support the individual post-identification. Some next steps may include3:
- Using FASD-informed practices and considerations to adapt practices that build on the strengths of your client, while acknowledging difficulties
- Forming partnerships and providing referrals to FASD assessment centres (for a list of available FASD clinics click here: FASD Diagnostic Clinics by Province)
- Connecting the individual with other appropriate supports and resources (e.g., employment, housing, medical needs)
FASD Assessment and Diagnostic Process
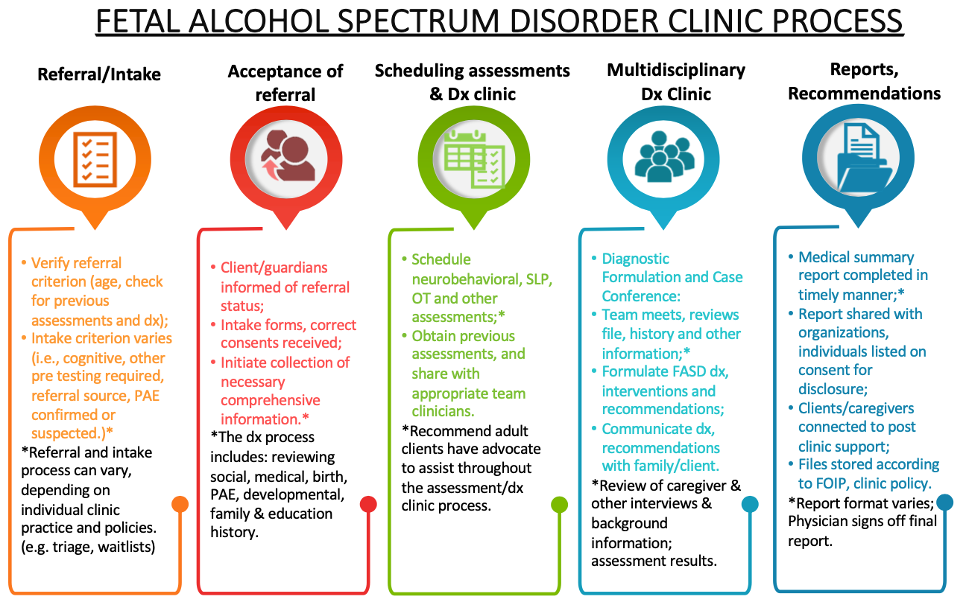
Assessments help to determine the strengths and challenges present for a person at that point in time and also help to understand what interventions and supports may be required1. The diagnostic process includes a multidisciplinary team examining a person’s full social and medical history, as well as a physical evaluation and neurodevelopmental and neuropsychological functional assessment by a psychologist, a speech language pathologist, and an occupation therapist2. After an assessment and diagnosis are completed, a report is developed outlining any diagnoses (which may include additional diagnoses that arise during the assessment), and recommendations for interventions and support.
The following flow chart provides an outline of what is typically involved in the Canadian FASD diagnostic clinic process (however, all clinics will have slightly varying processes; see FASD Diagnostic Clinic Process for full document)
As a mental health professional, you may be able to help your client through the diagnostic process in a variety of ways, including5:
-
-
- Confirming the number and the order of the appointments, the information required, and the other expectations of the individual
- Co-creating a schedule for the individual – discuss support with reminders or other needs about making it to appointments
- Providing emotional support to your client (e.g., actively listening to expectations, concerns, worries, etc.)
- Providing educational information about the impacts and potential benefits of the process and receiving a diagnosis
- Acting as a system navigator and providing guidance throughout the process
- Providing or arranging for transportation to and from appointments
- Identifying any financial support services that may be needed
- Referring to services that can be accessed without a diagnosis while waiting for a diagnosis
- Supporting the family and advocating for their needs
-
The Impact of Receiving a Diagnosis
There are a myriad of reasons why receiving a diagnosis can be beneficial for youth and adults. For youth, it can increase support available, allow for modifications or an individualized education plan in school, and can give parents and caregivers a better understanding of their youth’s behaviour, challenges, and strengths. Although it is a lot more challenging to receive a diagnosis as an adult, it can help people access health, education, and social services tailored to their needs1.
It is also important to acknowledge that receiving a diagnosis may create further problems for people, including being labeled, dealing with stigma, and possibly changing the way they are treated or held accountable for their actions. It is important to recognize that a diagnosis will mean something different to everyone; it may or may not be an important part of their identity and so having conversations about this consideration and meeting people where they are is important.
Children and Adolescents
As discussed, early diagnosis and appropriate intervention can be important mitigating factors for the onset of and/or severity of adverse health and psychosocial outcomes for people with FASD1. Obtaining an understanding of a child’s individual strengths, challenges, and neurodevelopmental presentation can help to support transitions, as well as intervention plans in the areas of health, education, and social services1. Depending on the age of the child, they may experience a variety of emotions including relief, sadness, anger, and/or confusion. Families may also struggle with the diagnosis, as well as with explaining it to their child.
Download Resource
For a downloadable resource for families on how to discuss FASD with their child: How to explain an FASD diagnosis to your child
Adults
There can be a variety of benefits for individuals who receive a FASD diagnosis as an adult, including improved access to support services, as well as disability income, developing a better understanding of areas of strengths and challenge, and empowerment through increasing their self-understanding and ability to advocate for their needs6. In a study examining adults receiving an FASD diagnosis it was expressed that:
Prior to a diagnosis, people may be unable to access income support as well as developmental disability support6. In addition, people with FASD have also reported that they were either indifferent to getting the diagnosis, or that they struggled with the idea of having FASD6. It is therefore important to understand what a diagnosis means to each person, and if you are working with someone engaging in the diagnostic process, it may be important to explore feelings of fear, anger, sadness, or concern for the future that may emerge6.
In the following video Reinier deSmit discusses the process of receiving a diagnosis as an adult: My Adult FASD Diagnosis: Nothing Changed. And Everything Changed.
Supporting People Without a Diagnosis
There are a myriad of reasons why receiving an FASD diagnosis may not be possible, or not wanted. For example, for adults, there is often not a clear way to obtain an assessment or individuals and families may be worried about stigma and the treatment they could experience post diagnosis. In addition, a diagnosis of FASD is not possible without a confirmation of prenatal alcohol exposure, and because of the stigma associated with alcohol use during pregnancy, parents may be hesitant to discuss or confirm this. In addition, it may not be possible to locate the birth mother/parent or another family member who could confirm the prenatal alcohol exposure required for diagnosis.
As a mental health worker, it is important to find ways to support the individual needs of your clients, regardless of a formal FASD diagnosis. If we approach everyone with a lens of accommodating their unique profile of strengths and challenges, we can better serve everyone we support, not just those with a labelled disability7. There are a variety of services and supports that are available and accessible without a diagnosis, that can be helpful to your clients, including: physical therapy, occupational therapy, and behavioural specialists.
Final Thoughts
The diagnostic process can impact people differently and as mental health professionals it is important to be aware of the impacts this may have on those we are supporting.
In the following video, Myles Himmelreich discusses how receiving a diagnosis has impacted his understanding of himself: Diagnosis: The start to a better understanding of FASD
Download Handout
For a summary of information, download the Mental Health Resource and Practice Guide Section 5 Summary.
References
1Green, C., Cook, J., & Salmon, A. (2015). Why is FASD diagnosis important? Vancouver (BC): CanFASD.
2Cook, J. L., Green, C. R., Lilley, C. M., Anderson, S. M., Baldwin, M. E., Chudley, A. E., Conry, J. L., LeBlanc, N., Loock, C. A., Lutke, J., Mallon, B. F., McFarlane, A. A., Temple, V. K., Rosales, T. (2016). Fetal alcohol spectrum disorder: a guideline for diagnosis across the lifespan. CMAJ: Canadian Medical Association journal, 188(3), 191–197. https://doi.org/10.1503/cmaj.141593
3Kapasi, A., Tremblay, M., Pei, J., Rorem, D., Makowecki, E., Wuest, V., Regier, M., McLachlan, K., Dunleavy, B., Mela, M., Benjamin, M., & DesRoches, A. (2022). Moving Towards FASD-Informed Care in Substance Use Treatment. Canada FASD Research Network.
4Wemigwans, J. (2008). FASD Tool Kit for Aboriginal Families. Ontario Federation of Indian Friendship Centres.
5CanFASD Online Training. CanFASD: FASD for Community and Social Services Professionals Level II. https://canfasd.ca/
6Temple, V. K., Prasad, S., Popova, S., & Lindsay, A. (2021). Long-term outcomes following Fetal Alcohol Spectrum Disorder (FASD) diagnosis in adulthood. Journal of Intellectual & Developmental Disability, 46(3), 272-280. http://dx.doi.org/10.3109/13668250.2020.1824612
7Harding, K., Pei, J. & Richardson, L. (2023). Neurodiversity and FASD. Canada FASD Research Network.
